Case of epigastric pain

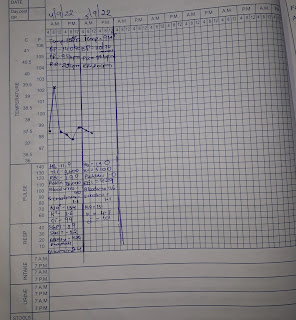
A 28 yr old male came to the opd with the following cheif complaints Cough since 5 days Epigastric pain since 3 days HISTORY OF PRESENTING ILLNESS The patient was apparently asymptomatic 5 days back.He developed cough since 5 days which was dry at the begginong and later it became productive. Since 3 days he developed pain in the epigastric region which was insidious in onset and gradually progressive in nature that aggaravated while coughing. Also has on and off episodes of fever. PAST HISTORY N/K/C/O DM, HTN, ASTHMA,TB,EPILEPSY PERSONAL HISTORY Diet - Mixed Appetite- decreased Bowel and bladder movements-passing urine regularly but did not pass stool for 2 days Sleep-adequate Addictions: consuming alcohol since 10 yrs initially occassionally but from 6 years started consuming daily ( 1 quarter) GENERAL EXAMINATION Patient is conscious coherent cooperative, well oriented to time ,place, person moderatly built and moderately nourished Pal...